Vaginismus
Vaginismus
| Vaginismus | |
|---|---|
| Other names | Vaginism, genito-pelvic pain disorder[1] |
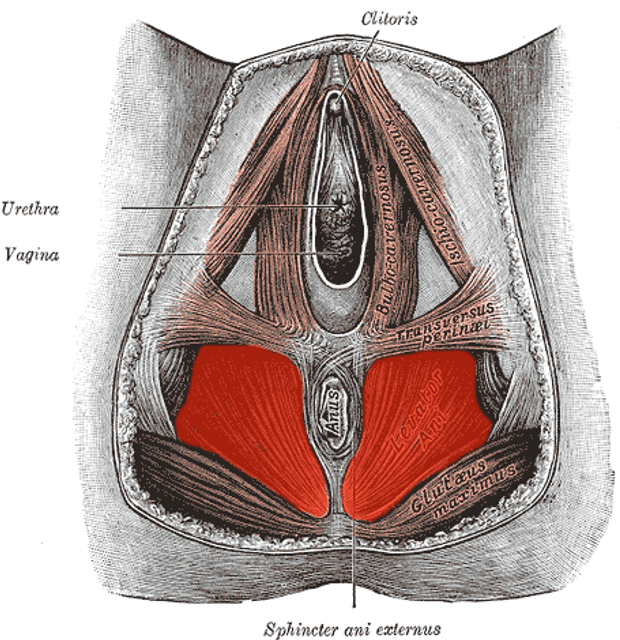
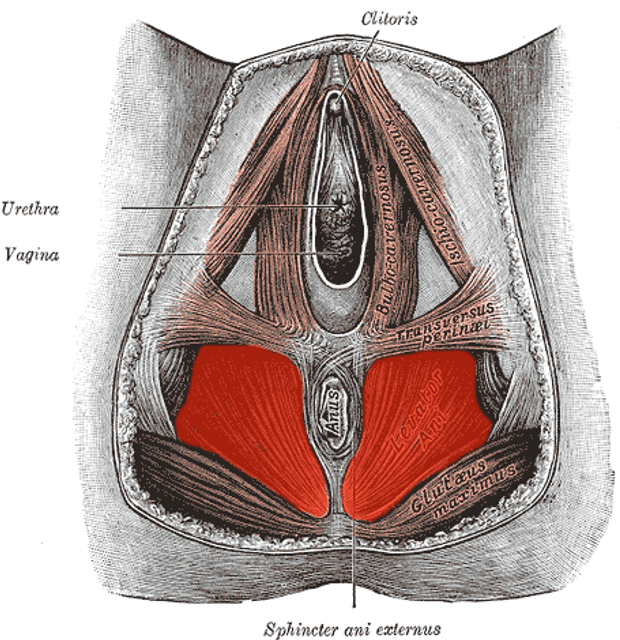
| Muscles included | |
| Specialty | Gynecology |
| Symptoms | Pain with sex[2] |
| Usual onset | With first sexual intercourse[3] |
| Causes | Fear of pain[3] |
| Risk factors | History of sexual assault, endometriosis, vaginitis, prior episiotomy[2] |
| Diagnostic method | Based on the symptoms and examination[2] |
| Differential diagnosis | Dyspareunia[4] |
| Treatment | Behavior therapy, gradual vaginal dilatation[2] |
| Prognosis | Generally good with treatment[5] |
| Frequency | 0.5% of women[2] |
Vaginismus is a condition in which involuntary muscle spasm prevents vaginal penetration.[2] This often results in pain with attempts at sex.[2] Often it begins when sexual intercourse is first attempted.[3]
The underlying cause is generally a fear that penetration will hurt.[3] Risk factors include a history of sexual assault, endometriosis, vaginitis, or a prior episiotomy.[2] Diagnosis is based on the symptoms and examination.[2] It requires there to be no anatomical or physical problems and a desire for penetration on the part of the woman.[3][6]
| Vaginismus | |
|---|---|
| Other names | Vaginism, genito-pelvic pain disorder[1] |
| Muscles included | |
| Specialty | Gynecology |
| Symptoms | Pain with sex[2] |
| Usual onset | With first sexual intercourse[3] |
| Causes | Fear of pain[3] |
| Risk factors | History of sexual assault, endometriosis, vaginitis, prior episiotomy[2] |
| Diagnostic method | Based on the symptoms and examination[2] |
| Differential diagnosis | Dyspareunia[4] |
| Treatment | Behavior therapy, gradual vaginal dilatation[2] |
| Prognosis | Generally good with treatment[5] |
| Frequency | 0.5% of women[2] |
Signs and symptoms
Severity and pain during vaginal penetration varies.[7]
Causes
Primary vaginismus
Vaginismus occurs when penetrative sex or other vaginal penetration cannot be experienced without pain. It is commonly discovered among teenage girls and women in their early twenties, as this is when many girls and young women first attempt to use tampons, have penetrative sex, or undergo a Pap smear. Awareness of vaginismus may not happen until vaginal penetration is attempted. Reasons for the condition may be unknown.[[8]](https://portal.issn.org/resource/ISSN/"Botox treatment for vaginismus")
A few of the main factors that may contribute to primary vaginismus include:
a condition called vulvar vestibulitis syndrome, more or less synonymous with focal vaginitis, a so-called sub-clinical inflammation, in which no pain is perceived until some form of penetration is attempted
urinary tract infections
vaginal yeast infections
sexual abuse, rape, other sexual assault, or attempted sexual abuse or assault
knowledge of (or witnessing) sexual or physical abuse of others, without being personally abused
domestic violence or similar conflict in the early home environment
fear of pain associated with penetration, particularly the popular misconception of "breaking" the hymen upon the first attempt at penetration, or the idea that vaginal penetration will inevitably hurt the first time it occurs
chronic pain conditions and harm-avoidance behaviour[9]
any physically invasive trauma (not necessarily involving or even near the genitals)
generalized anxiety
stress
negative emotional reaction towards sexual stimulation, e.g. disgust both at a deliberate level and also at a more implicit level[10]
strict conservative moral education, which also can elicit negative emotions[11]
Primary vaginismus is often idiopathic.[12]
Vaginismus has been classified by Lamont[13] according to the severity of the condition. Lamont describes four degrees of vaginismus: In first degree vaginismus, the person has spasm of the pelvic floor that can be relieved with reassurance. In second degree, the spasm is present but maintained throughout the pelvis even with reassurance. In third degree, the people elevates the buttocks to avoid being examined. In fourth degree vaginismus (also known as grade 4 vaginismus), the most severe form of vaginismus, the person elevates the buttocks, retreats and tightly closes the thighs to avoid examination. Pacik expanded the Lamont classification to include a fifth degree in which the person experiences a visceral reaction such as sweating, hyperventilation, palpitations, trembling, shaking, nausea, vomiting, losing consciousness, wanting to jump off the table, or attacking the doctor.[14] The Lamont classification continues to be used to the present and allows for a common language among researchers and therapists.
Although the pubococcygeus muscle is commonly thought to be the primary muscle involved in vaginismus, Pacik identified two additionally-involved spastic muscles in people who were treated under sedation. These include the entry muscle (bulbocavernosum) and the mid-vaginal muscle (puborectalis). Spasm of the entry muscle accounts for the common complaint that people often report when trying to have intercourse: "It's like hitting a brick wall".[[8]](https://portal.issn.org/resource/ISSN/"Botox treatment for vaginismus")
Secondary vaginismus
Secondary vaginismus occurs when a person who has previously been able to achieve penetration develops vaginismus. This may be due to physical causes such as a yeast infection or trauma during childbirth, while in some cases it may be due to psychological causes, or to a combination of causes. The treatment for secondary vaginismus is the same as for primary vaginismus, although, in these cases, previous experience with successful penetration can assist in a more rapid resolution of the condition. Peri-menopausal and menopausal vaginismus, often due to a drying of the vulvar and vaginal tissues as a result of reduced estrogen, may occur as a result of "micro-tears" first causing sexual pain then leading to vaginismus.[15]
Further factors that may contribute to either secondary or primary vaginismus include:
Fear of losing control
Not trusting one’s partner
Self-consciousness about body image
History of sexual abuse, rape, sexual assault, or attempted sexual abuse or assault
Misconceptions about sex or unattainable standards for sex from exaggerated sexual materials, such as pornography or abstinence
Fear of vagina not being wide or deep enough / fear of partner’s penis being too large
Undiscovered or denied sexuality
Mechanism
Which muscles are involved is unclear but may include the pubococcygeus muscle, levator ani, bulbocavernosus, circumvaginal, and perivaginal muscles.[16]
Diagnosis
The diagnosis of vaginismus, as well as other diagnoses of female sexual dysfunction, can be made when "symptoms are sufficient to result in personal distress."[17] The DSM-IV-TR defines vaginismus as "recurrent or persistent involuntary spasm of the musculature of the outer third of the vagina that interferes with sexual intercourse, causing marked distress or interpersonal difficulty".[17]
Treatment
Psychological
According to Ward and Ogden's qualitative study on the experience of vaginismus (1994), the three most common contributing factors to vaginismus are fear of painful sex; the belief that sex is wrong or shameful (often the case with people who had a strict religious upbringing); and traumatic early childhood experiences (not necessarily sexual in nature).
Those with vaginismus are twice as likely to have a history of childhood sexual interference and held less positive attitudes about their sexuality, whereas no correlation was noted for lack of sexual knowledge or (non-sexual) physical abuse.[19]
Physical

Dilators for treating vaginismus
Often, when faced with a person experiencing painful intercourse, a gynecologist will recommend Kegel exercises and provide some additional lubricants.[20][21][22][23] Strengthening the muscles that unconsciously tighten during vaginismus may be extremely counter-intuitive for some people. Although vaginismus has not been shown to affect a person's ability to produce lubrication, providing additional lubricant can be helpful in achieving successful penetration. This is due to the fact that women may not produce natural lubrication if anxious or in pain. Treatment of vaginismus may involve the use Hegar dilators, (sometimes called vaginal trainers[24]) progressively increasing the size of the dilator inserted into the vagina.[25]
Neuromodulators
Botulinum toxin A (Botox) has been considered as a treatment option, under the idea of temporarily reducing the hypertonicity of the pelvic floor muscles. Although no random controlled trials have been done with this treatment, experimental studies with small samples have shown it to be effective, with sustained positive results through 10 months.[16][26] Similar in its mechanism of treatment, lidocaine has also been tried as an experimental option.[16][27]
Epidemiology
True epidemiological studies of vaginismus have not been done, as diagnosis would require painful examinations that those with vaginismus would most likely avoid. Data available is primarily reported statistics from clinical settings.[16]
A study of vaginismus in Morocco and Sweden found a rate of 6%. 18-20% of people in British and Australian studies were found to have manifest dyspareunia, while the rate among elderly British people was as low as 2%.[28]
A 1990 study of people presenting to sex therapy clinics found reported vaginismus rates of between 12% and 17%, while a random sampling and structured interview survey conducted in 1994 by National Health and Sexual Life Survey documented a 10%-15% rate of painful sexual intercourse in the past six months, but did not differentiate between vaginismus and dyspareunia.[12]
The most recent study-based estimates of vaginismus cases range from 5% to 47% of those presenting for sex therapy or complaining of sexual problems, with significant differences across cultures.[29] It seems likely that a society's expectations of person's sexuality may particularly impact on those with the vaginismus.[30]
See also
Penis captivus
Vulvodynia