Ewing's sarcoma
Ewing's sarcoma
| Ewing's sarcoma | |
|---|---|
| Other names | Ewing sarcoma, peripheral primitive neuroectodermal tumor, Askin tumor, and Ewing sarcoma family of tumors[1] |
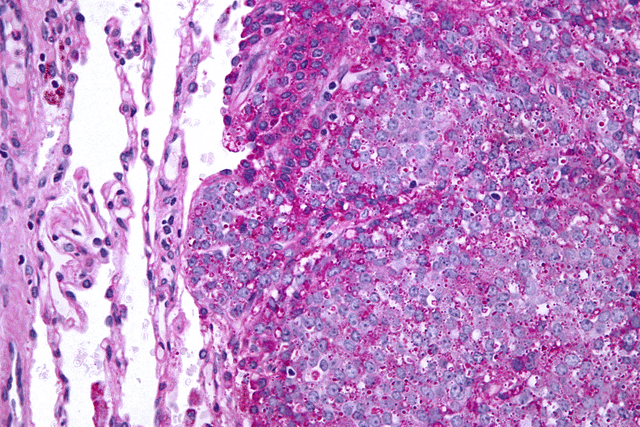
| Micrograph of metastatic Ewing sarcoma (right of image) in normal lung (left of image). PAS stain. | |
| Pronunciation |
|
| Specialty | Oncology |
| Symptoms | Swell and pain near the tumor[1] |
| Complications | Pleural effusion, paraplegia[2] |
| Usual onset | 10 to 20 years old[3][2] |
| Causes | Unknown[2] |
| Diagnostic method | Tissue biopsy[1] |
| Differential diagnosis | Osteosarcoma, neuroblastoma, osteomyelitis, eosinophilic granuloma[2] |
| Treatment | Chemotherapy, radiation therapy, surgery, stem cell transplant[1] |
| Prognosis | Five year survival ~ 70%[3] |
| Frequency | 1 per million people (US)[3] |
Ewing's sarcoma is a type of cancer that forms in bone or soft tissue.[1] Symptoms may include swelling and pain at the site of the tumor, fever, and a bone fracture.[1] The most common areas where it begins are the legs, pelvis, and chest wall.[3] In about 25% of cases, the cancer has already spread to other parts of the body at the time of diagnosis.[3] Complications may include a pleural effusion or paraplegia.[2]
The cause of Ewing's sarcoma is unknown.[2] Most cases appear to occur randomly.[2] It is sometimes grouped together with primitive neuroectodermal tumors, in a category known as the Ewing family of tumors.[2] The underlying mechanism often involves a genetic change known as a reciprocal translocation.[2] Diagnosis is based on biopsy of the tumor.[1]
Treatment often includes chemotherapy, radiation therapy, surgery, and stem cell transplant.[1] Targeted therapy and immunotherapy are being studied.[1] Five year survival is about 70%.[3] A number of factors, however, affect this estimate.[3]
James Ewing in 1920 established that the tumor is a distinct type of cancer.[4][5] It affects about one in a million people per year in the United States.[3] Ewing's sarcoma occurs most often in teenagers and young adults and represents 2% of childhood cancers.[1][2] Caucasians are affected more often than African Americans or Asians.[3] Males are affected more often than females.[3]
| Ewing's sarcoma | |
|---|---|
| Other names | Ewing sarcoma, peripheral primitive neuroectodermal tumor, Askin tumor, and Ewing sarcoma family of tumors[1] |
| Micrograph of metastatic Ewing sarcoma (right of image) in normal lung (left of image). PAS stain. | |
| Pronunciation |
|
| Specialty | Oncology |
| Symptoms | Swell and pain near the tumor[1] |
| Complications | Pleural effusion, paraplegia[2] |
| Usual onset | 10 to 20 years old[3][2] |
| Causes | Unknown[2] |
| Diagnostic method | Tissue biopsy[1] |
| Differential diagnosis | Osteosarcoma, neuroblastoma, osteomyelitis, eosinophilic granuloma[2] |
| Treatment | Chemotherapy, radiation therapy, surgery, stem cell transplant[1] |
| Prognosis | Five year survival ~ 70%[3] |
| Frequency | 1 per million people (US)[3] |
Signs and symptoms
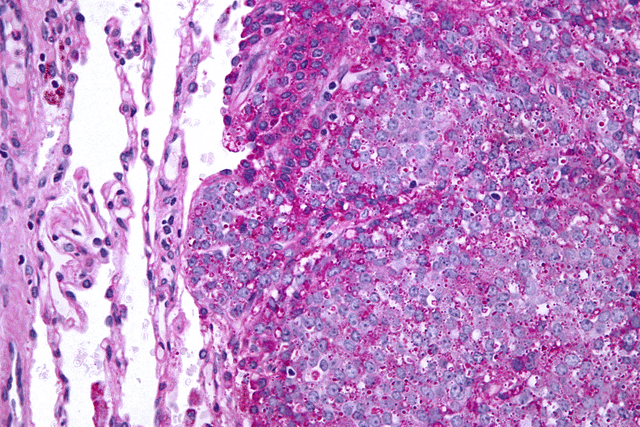
Distribution of Ewing's sarcoma: Most frequent locations are the large long bones and the pelvis.
Ewing's sarcoma is more common in males (1.6 male:1 female) and usually presents in childhood or early adulthood, with a peak between 10 and 20 years of age. It can occur anywhere in the body, but most commonly in the pelvis and proximal long tubular bones, especially around the growth plates. The diaphyses of the femur are the most common sites, followed by the tibia and the humerus. Thirty percent are overtly metastatic at presentation. People usually experience extreme bone pain. Rarely, it can develop in the vagina.[6][7]
According to the Bone Cancer Research Trust (BCRT), the most common symptoms are: localized pain, swelling, and sporadic bone pain with variable intensity. The swelling is most likely to be visible if the sarcoma is located on a bone near the surface of the body, but when it occurs in other places deeper in the body, like on the pelvis, it may not be visible.[9]
Causes
Genetic exchange between chromosomes can cause cells to become cancerous. Most cases of Ewing's sarcoma (85%) are the result of a translocation between chromosomes 11 and 22, which fuses the EWS gene of chromosome 22 to the FLI1 gene of chromosome 11.[8]
Diagnosis
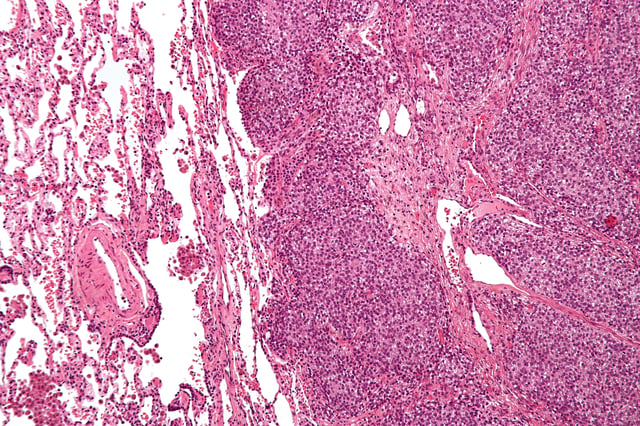
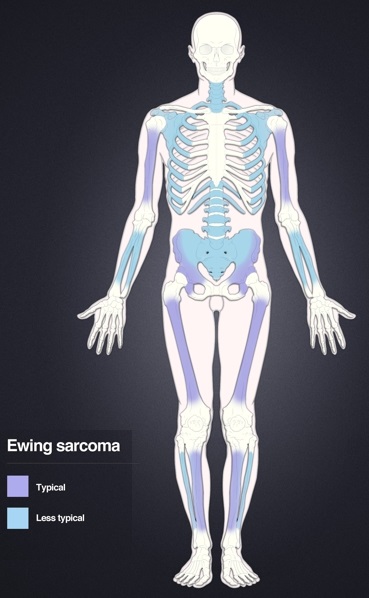
Micrograph of a metastatic Ewing's sarcoma with the characteristic cytoplasmic clearing on H&E staining, which was showing to be PAS positive.
The definitive diagnosis is based on histomorphologic findings, immunohistochemistry and molecular pathology.
Ewing's sarcoma is a small-blue-round-cell tumor that typically has a clear cytoplasm on H&E staining, due to glycogen. The presence of the glycogen can be demonstrated with positive PAS staining and negative PAS diastase staining. The characteristic immunostain is CD99, which diffusely marks the cell membrane. However, as CD99 is not specific for Ewing's sarcoma, several auxiliary immunohistochemical markers can be employed to support the histological diagnosis.[14][15] Morphologic and immunohistochemical findings are corroborated with an associated chromosomal translocation, of which several occur. The most common translocation, present in about 90% of Ewing sarcoma cases, is t(11;22)(q24;q12),[16][17] which generates an aberrant transcription factor through fusion of the EWSR1 gene with the FLI1 gene.[18]
The pathologic differential diagnosis is the grouping of small-blue-round-cell tumors, which includes lymphoma, alveolar rhabdomyosarcoma, and desmoplastic small round cell tumor, among others.
Medical imaging

X-ray of a child with Ewing's sarcoma of the tibia

Magnetic resonance imaging slice showing Ewing's sarcoma of the left hip (white area shown right)
On conventional radiographs, the most common osseous presentation is a permeative lytic lesion with periosteal reaction. The classic description of lamellated or "onion-skin" type periosteal reaction is often associated with this lesion. Plain films add valuable information in the initial evaluation or screening. The wide zone of transition (e.g. permeative) is the most useful plain film characteristic in differentiation of benign versus aggressive or malignant lytic lesions.
Magnetic resonance imaging (MRI) should be routinely used in the work-up of malignant tumors. It will show the full bony and soft tissue extent and relate the tumor to other nearby anatomic structures (e.g. vessels). Gadolinium contrast is not necessary as it does not give additional information over noncontrast studies, though some current researchers argue that dynamic, contrast-enhanced MRI may help determine the amount of necrosis within the tumor, thus help in determining response to treatment prior to surgery.
Computed axial tomography(CT) can also be used to define the extraosseous extent of the tumor, especially in the skull, spine, ribs, and pelvis. Both CT and MRI can be used to follow response to radiation and/or chemotherapy. Bone scintigraphy can also be used to follow tumor response to therapy.
In the group of malignant small round cell tumors which include Ewing's sarcoma, bone lymphoma, and small cell osteosarcoma, the cortex may appear almost normal radiographically, while permeative growth occurs throughout the Haversian channels. These tumours may be accompanied by a large soft-tissue mass while almost no bone destruction is visible. The radiographs frequently do not shown any signs of cortical destruction.
Radiographically, Ewing's sarcoma presents as "moth-eaten" destructive radiolucencies of the medulla and erosion of the cortex with expansion.
Differential diagnosis
Other entities with similar clinical presentations include osteomyelitis, osteosarcoma (especially telangiectatic osteosarcoma), and eosinophilic granuloma. Soft-tissue neoplasms such as pleomorphic undifferentiated sarcoma (malignant fibrous histiocytoma) that erode into adjacent bone may also have a similar appearance. Accumulating evidence suggests that EWSR1-NFATc2 positive sarcomas, which were previously considered to possibly belong to the Ewing family of tumors, differ from Ewing's sarcoma in their genetics, transcriptomes, epigentic and epidemiological profiles, indicating that they might represent a distinct tumor entity.[19][20][21][22][23]
Treatment
Almost all patients require multidrug chemotherapy (often including ifosfamide and etoposide),[24] as well as local disease control with surgery and/or radiation.[25] An aggressive approach is necessary because almost all patients with apparently localized disease at the time of diagnosis actually have asymptomatic metastatic disease.
The surgical resection may involve limb salvage or amputation. Complete excision at the time of biopsy may be performed if malignancy is confirmed at the time it is examined. Treatment lengths vary depending on location and stage of the disease at diagnosis. Radical chemotherapy may be as short as six treatments at 3-week cycles, but most patients undergo chemotherapy for 6–12 months and radiation therapy for 5–8 weeks. Radiotherapy has been used for localized disease. The tumor has a unique property of being highly sensitive to radiation, sometimes acknowledged by the phrase "melting like snow", but the main drawback is that it recurs dramatically after some time.
Antisense oligodeoxynucleotides have been proposed as possible treatment by down-regulating the expression of the oncogenic fusion protein associated with the development of Ewing's sarcoma resulting from the EWS-ETS gene translocation.[26][27] In addition, the synthetic retinoid derivative fenretinide (4-hydroxy(phenyl)retinamide) has been reported to induce high levels of cell death in Ewing's sarcoma cell lines in vitro and to delay growth of xenografts in in vivo mouse models.[28][29]
In most pediatric cancers including sarcoma, proton beam radiation (also known as proton therapy) delivers an equally effective dose to the tumor with less damage to the surrounding normal tissue compared to photon radiation.[30]
Prognosis
Staging attempts to distinguish patients with localized from those with metastatic disease.[31] Most commonly, metastases occur in the chest, bone and/or bone marrow. Less common sites include the central nervous system and lymph nodes.
Five-year survival for localized disease is 70% to 80% when treated with chemotherapy.[32] Prior to the use of multi-drug chemotherapy, long-term survival was less than 10%. The development of multi-disciplinary therapy with chemotherapy, irradiation, and surgery has increased current long-term survival rates in most clinical centers to greater than 50%.[33] However, some sources state it is 25–30%.[34]
Retrospective research in patients led by Idriss M. Bennani-Baiti (Cancer Epigenetics Society) showed that two chemokine receptors, CXCR4 and CXCR7, can be used as molecular prognosis factors. Patients who express low levels of both chemokine receptors have the highest odds of long-term survival with >90% survival at 5 years post-diagnosis versus <30% survival at 5 years for patients with very high expression levels of both receptors.[35] A recent study also suggested a role for SOX2 as an independent prognostic biomarker that can be used to identify patients at high risk for tumor relapse.[36]
Epidemiology
Ewing's sarcomas represent 16% of primary bone sarcomas.[8] In the United States, they are most common in the second decade of life,[8] with a rate of 0.3 cases per million in children under 3 years of age, and as high as 4.6 cases per million in adolescents aged 15–19 years. Internationally, the annual incidence rate averages less than 2 cases per million children.[37]
In the United Kingdom, an average of six children per year are diagnosed, mainly males in early stages of puberty. Due to the prevalence of diagnosis during teenage years, a link may exist between the onset of puberty and the early stages of this disease, although no research confirms this hypothesis.
A grouping of three unrelated teenagers in Wake Forest, NC, have been diagnosed with Ewing's sarcoma. All three children were diagnosed in 2011 and all attended the same temporary classroom together while the school underwent renovation. A fourth teenager living nearby was diagnosed in 2009. The odds of this grouping are considered significant.[38]
Ewing's sarcoma occurs about 10- to 20-fold more commonly in people of European descent as compared to people from African descent.[39] Consistently, a genome-wide association study (GWAS) conducted in several hundred European individuals with Ewing's sarcoma and genetically-matched healthy controls identified three susceptibility loci located on chromosomes 1, 10 and 15.[40] A continuative study discovered that the Ewing's sarcoma susceptibility gene EGR2, which is located within the chromosome 10 susceptibility locus, is regulated by the EWSR1-FLI1 fusion oncogene via a GGAA-microsatellite.[41][42]
Ewing's sarcoma is the second most common bone cancer in children and adolescents, with poor prognosis and outcome in ~70% of initial diagnoses and 10–15% of relapses.[43]