Autism

Autism

| Autism | |
|---|---|
| Repetitively stacking or lining up objects is associated with autism. | |
| Specialty | Psychiatry |
| Symptoms | Trouble with social interaction, impaired communication, restricted interests, repetitive behavior[1] |
| Complications | Social isolation, employment problems, family stress, bullying[2] |
| Usual onset | By age two or three[3][4] |
| Duration | Long-term[3] |
| Causes | Genetic and environmental factors[5] |
| Diagnostic method | Based on behavior and developmental history[3] |
| Differential diagnosis | Reactive attachment disorder, intellectual disability, schizophrenia[6] |
| Treatment | Behavioral therapy, speech therapy, psychotropic medication[7][8][9] |
| Medication | Antipsychotics, antidepressants, stimulants (associated symptoms)[10][11][12] |
| Prognosis | Frequently poor[13] |
| Frequency | 24.8 million (2015)[14] |
Autism is a developmental disorder characterized by difficulties with social interaction and communication, and by restricted and repetitive behavior.[4] Parents usually notice signs during the first three years of their child's life.[1][4] These signs often develop gradually, though some children with autism reach their developmental milestones at a normal pace before worsening.[15]
Autism is associated with a combination of genetic and environmental factors.[5] Risk factors during pregnancy include certain infections, such as rubella, toxins including valproic acid, alcohol, cocaine, pesticides and air pollution, fetal growth restriction, and autoimmune diseases.[16][17][18] Controversies surround other proposed environmental causes; for example, the vaccine hypothesis, which has been effectively dismissed.[19] Autism affects information processing in the brain by altering connections and organization of nerve cells and their synapses.[20] How this occurs is not well understood.[20] In the DSM-5, autism and less severe forms of the condition, including Asperger syndrome and pervasive developmental disorder not otherwise specified (PDD-NOS), have been combined into the diagnosis of autism spectrum disorder (ASD).[4][21]
Early behavioral interventions or speech therapy can help children with autism gain self-care, social, and communication skills.[7][8] Although there is no known cure,[7] there have been cases of children who recovered.[22] Not many children with autism live independently after reaching adulthood, though some are successful.[13] An autistic culture has developed, with some individuals seeking a cure and others believing autism should be accepted as a difference and not treated as a disorder.[23][24]
Globally, autism is estimated to affect 24.8 million people as of 2015.[14] In the 2000s, the number of people affected was estimated at 1–2 per 1,000 people worldwide.[25] In the developed countries, about 1.5% of children are diagnosed with ASD as of 2017.[26] from 0.7% in 2000 in the United States.[27] It occurs four-to-five times more often in males than females.[27] The number of people diagnosed has increased dramatically since the 1960s, which may be partly due to changes in diagnostic practice.[25] The question of whether actual rates have increased is unresolved.[25]
| Autism | |
|---|---|
| Repetitively stacking or lining up objects is associated with autism. | |
| Specialty | Psychiatry |
| Symptoms | Trouble with social interaction, impaired communication, restricted interests, repetitive behavior[1] |
| Complications | Social isolation, employment problems, family stress, bullying[2] |
| Usual onset | By age two or three[3][4] |
| Duration | Long-term[3] |
| Causes | Genetic and environmental factors[5] |
| Diagnostic method | Based on behavior and developmental history[3] |
| Differential diagnosis | Reactive attachment disorder, intellectual disability, schizophrenia[6] |
| Treatment | Behavioral therapy, speech therapy, psychotropic medication[7][8][9] |
| Medication | Antipsychotics, antidepressants, stimulants (associated symptoms)[10][11][12] |
| Prognosis | Frequently poor[13] |
| Frequency | 24.8 million (2015)[14] |
Characteristics
Autism is a highly variable, neurodevelopmental disorder[28] whose symptoms first appears during infancy or childhood, and generally follows a steady course without remission.[29] People with autism may be severely impaired in some respects but normal, or even superior, in others.[30] Overt symptoms gradually begin after the age of six months, become established by age two or three years[31] and tend to continue through adulthood, although often in more muted form.[32] It is distinguished not by a single symptom but by a characteristic triad of symptoms: impairments in social interaction; impairments in communication; and restricted interests and repetitive behavior. Other aspects, such as atypical eating, are also common but are not essential for diagnosis.[33] Individual symptoms of autism occur in the general population and appear not to associate highly, without a sharp line separating pathologically severe from common traits.[34]
Social development
Social deficits distinguish autism and the related autism spectrum disorders (ASD; see Classification) from other developmental disorders.[32] People with autism have social impairments and often lack the intuition about others that many people take for granted. Noted autistic Temple Grandin described her inability to understand the social communication of neurotypicals, or people with normal neural development, as leaving her feeling "like an anthropologist on Mars".[35]
Unusual social development becomes apparent early in childhood. Autistic infants show less attention to social stimuli, smile and look at others less often, and respond less to their own name. Autistic toddlers differ more strikingly from social norms; for example, they have less eye contact and turn-taking, and do not have the ability to use simple movements to express themselves, such as pointing at things.[36] Three- to five-year-old children with autism are less likely to exhibit social understanding, approach others spontaneously, imitate and respond to emotions, communicate nonverbally, and take turns with others. However, they do form attachments to their primary caregivers.[37] Most children with autism display moderately less attachment security than neurotypical children, although this difference disappears in children with higher mental development or less severe ASD.[38] Older children and adults with ASD perform worse on tests of face and emotion recognition[39] although this may be partly due to a lower ability to define a person's own emotions.[40]
Children with high-functioning autism suffer from more intense and frequent loneliness compared to non-autistic peers, despite the common belief that children with autism prefer to be alone. Making and maintaining friendships often proves to be difficult for those with autism. For them, the quality of friendships, not the number of friends, predicts how lonely they feel. Functional friendships, such as those resulting in invitations to parties, may affect the quality of life more deeply.[41]
There are many anecdotal reports, but few systematic studies, of aggression and violence in individuals with ASD. The limited data suggest that, in children with intellectual disability, autism is associated with aggression, destruction of property, and meltdowns.[42]
Communication
About a third to a half of individuals with autism do not develop enough natural speech to meet their daily communication needs.[43] Differences in communication may be present from the first year of life, and may include delayed onset of babbling, unusual gestures, diminished responsiveness, and vocal patterns that are not synchronized with the caregiver. In the second and third years, children with autism have less frequent and less diverse babbling, consonants, words, and word combinations; their gestures are less often integrated with words. Children with autism are less likely to make requests or share experiences, and are more likely to simply repeat others' words (echolalia)[44][45] or reverse pronouns.[46] Joint attention seems to be necessary for functional speech, and deficits in joint attention seem to distinguish infants with ASD.[21] For example, they may look at a pointing hand instead of the pointed-at object,[36][45] and they consistently fail to point at objects in order to comment on or share an experience.[21] Children with autism may have difficulty with imaginative play and with developing symbols into language.[44][45]
In a pair of studies, high-functioning children with autism aged 8–15 performed equally well as, and as adults better than, individually matched controls at basic language tasks involving vocabulary and spelling. Both autistic groups performed worse than controls at complex language tasks such as figurative language, comprehension and inference. As people are often sized up initially from their basic language skills, these studies suggest that people speaking to autistic individuals are more likely to overestimate what their audience comprehends.[47]
Repetitive behavior

A young boy with autism who has arranged his toys in a row
Autistic individuals can display many forms of repetitive or restricted behavior, which the Repetitive Behavior Scale-Revised (RBS-R) categorizes as follows.[48]
Stereotyped behaviors: Repetitive movements, such as hand flapping, head rolling, or body rocking.
Compulsive behaviors: Time-consuming behaviors intended to reduce anxiety that an individual feels compelled to perform repeatedly or according to rigid rules, such as placing objects in a specific order, checking things, or hand washing.
Sameness: Resistance to change; for example, insisting that the furniture not be moved or refusing to be interrupted.
Ritualistic behavior: Unvarying pattern of daily activities, such as an unchanging menu or a dressing ritual. This is closely associated with sameness and an independent validation has suggested combining the two factors.[48]
Restricted interests: Interests or fixations that are abnormal in theme or intensity of focus, such as preoccupation with a single television program, toy, or game.
Self-injury: Behaviors such as eye-poking, skin-picking, hand-biting and head-banging.[21]
No single repetitive or self-injurious behavior seems to be specific to autism, but autism appears to have an elevated pattern of occurrence and severity of these behaviors.[49]
Other symptoms
Autistic individuals may have symptoms that are independent of the diagnosis, but that can affect the individual or the family.[33] An estimated 0.5% to 10% of individuals with ASD show unusual abilities, ranging from splinter skills such as the memorization of trivia to the extraordinarily rare talents of prodigious autistic savants.[50] Many individuals with ASD show superior skills in perception and attention, relative to the general population.[51] Sensory abnormalities are found in over 90% of those with autism, and are considered core features by some,[52] although there is no good evidence that sensory symptoms differentiate autism from other developmental disorders.[53] Differences are greater for under-responsivity (for example, walking into things) than for over-responsivity (for example, distress from loud noises) or for sensation seeking (for example, rhythmic movements).[54] An estimated 60–80% of autistic people have motor signs that include poor muscle tone, poor motor planning, and toe walking;[52] deficits in motor coordination are pervasive across ASD and are greater in autism proper.[55] Unusual eating behavior occurs in about three-quarters of children with ASD, to the extent that it was formerly a diagnostic indicator. Selectivity is the most common problem, although eating rituals and food refusal also occur.[56]
Parents of children with ASD have higher levels of stress.[36] Siblings of children with ASD report greater admiration of and less conflict with the affected sibling than siblings of unaffected children and were similar to siblings of children with Down syndrome in these aspects of the sibling relationship. However, they reported lower levels of closeness and intimacy than siblings of children with Down syndrome; siblings of individuals with ASD have greater risk of negative well-being and poorer sibling relationships as adults.[57] There is tentative evidence that autism occurs more frequently in people with gender dysphoria.[58][59]
Causes

Deletion (1), duplication (2) and inversion (3) are all chromosome abnormalities that have been implicated in autism.[64]
It has long been presumed that there is a common cause at the genetic, cognitive, and neural levels for autism's characteristic triad of symptoms.[62] However, there is increasing suspicion that autism is instead a complex disorder whose core aspects have distinct causes that often co-occur.[62][63]
Autism has a strong genetic basis, although the genetics of autism are complex and it is unclear whether ASD is explained more by rare mutations with major effects, or by rare multigene interactions of common genetic variants.[65][66] Complexity arises due to interactions among multiple genes, the environment, and epigenetic factors which do not change DNA sequencing but are heritable and influence gene expression.[32] Many genes have been associated with autism through sequencing the genomes of affected individuals and their parents.[67] Studies of twins suggest that heritability is 0.7 for autism and as high as 0.9 for ASD, and siblings of those with autism are about 25 times more likely to be autistic than the general population.[52] However, most of the mutations that increase autism risk have not been identified. Typically, autism cannot be traced to a Mendelian (single-gene) mutation or to a single chromosome abnormality, and none of the genetic syndromes associated with ASDs have been shown to selectively cause ASD.[65] Numerous candidate genes have been located, with only small effects attributable to any particular gene.[65] Most loci individually explain less than 1% of cases of autism.[68] The large number of autistic individuals with unaffected family members may result from spontaneous structural variation — such as deletions, duplications or inversions in genetic material during meiosis.[69][70] Hence, a substantial fraction of autism cases may be traceable to genetic causes that are highly heritable but not inherited: that is, the mutation that causes the autism is not present in the parental genome.[64] Autism may be underdiagnosed in women and girls due to an assumption that it is primarily a male condition,[71] but genetic phenomena such as imprinting and X linkage have the ability to raise the frequency and severity of conditions in males, and theories have been put forward for a genetic reason why males are diagnosed more often, such as the imprinted brain theory and the extreme male brain theory.[72][73][74]
Maternal nutrition and inflammation during preconception and pregnancy influences fetal neurodevelopment. Intrauterine growth restriction is associated with ASD, in both term and preterm infants.[17] Maternal inflammatory and autoimmune diseases may damage fetal tissues, aggravating a genetic problem or damaging the nervous system.[18]
Exposure to air pollution during pregnancy, especially heavy metals and particulates, may increase the risk of autism.[75][76] Environmental factors that have been claimed without evidence to contribute to or exacerbate autism include certain foods, infectious diseases, solvents, PCBs, phthalates and phenols used in plastic products, pesticides, brominated flame retardants, alcohol, smoking, illicit drugs, vaccines,[25] and prenatal stress. Some, such as the MMR vaccine, have been completely disproven.[77][78][79]
Parents may first become aware of autistic symptoms in their child around the time of a routine vaccination. This has led to unsupported theories blaming vaccine "overload", a vaccine preservative, or the MMR vaccine for causing autism.[80] The latter theory was supported by a litigation-funded study that has since been shown to have been "an elaborate fraud".[81] Although these theories lack convincing scientific evidence and are biologically implausible,[80] parental concern about a potential vaccine link with autism has led to lower rates of childhood immunizations, outbreaks of previously controlled childhood diseases in some countries, and the preventable deaths of several children.[82][83]
Mechanism
Autism's symptoms result from maturation-related changes in various systems of the brain. How autism occurs is not well understood. Its mechanism can be divided into two areas: the pathophysiology of brain structures and processes associated with autism, and the neuropsychological linkages between brain structures and behaviors.[84] The behaviors appear to have multiple pathophysiologies.[34]
There is evidence that gut–brain axis abnormalities may be involved.[61][85][60] A 2015 review proposed that immune dysregulation, gastrointestinal inflammation, malfunction of the autonomic nervous system, gut flora alterations, and food metabolites may cause brain neuroinflammation and dysfunction.[61] A 2016 review concludes that enteric nervous system abnormalities might play a role in neurological disorders such as autism. Neural connections and the immune system are a pathway that may allow diseases originated in the intestine to spread to the brain.[85]
Several lines of evidence point to synaptic dysfunction as a cause of autism.[20] Some rare mutations may lead to autism by disrupting some synaptic pathways, such as those involved with cell adhesion.[86] Gene replacement studies in mice suggest that autistic symptoms are closely related to later developmental steps that depend on activity in synapses and on activity-dependent changes.[87] All known teratogens (agents that cause birth defects) related to the risk of autism appear to act during the first eight weeks from conception, and though this does not exclude the possibility that autism can be initiated or affected later, there is strong evidence that autism arises very early in development.[88]
Diagnosis
Diagnosis is based on behavior, not cause or mechanism.[34][89] Under the DSM-5, autism is characterized by persistent deficits in social communication and interaction across multiple contexts, as well as restricted, repetitive patterns of behavior, interests, or activities. These deficits are present in early childhood, typically before age three, and lead to clinically significant functional impairment.[4] Sample symptoms include lack of social or emotional reciprocity, stereotyped and repetitive use of language or idiosyncratic language, and persistent preoccupation with unusual objects. The disturbance must not be better accounted for by Rett syndrome, intellectual disability or global developmental delay.[4] ICD-10 uses essentially the same definition.[29]
Several diagnostic instruments are available. Two are commonly used in autism research: the Autism Diagnostic Interview-Revised (ADI-R) is a semistructured parent interview, and the Autism Diagnostic Observation Schedule (ADOS)[90] uses observation and interaction with the child. The Childhood Autism Rating Scale (CARS) is used widely in clinical environments to assess severity of autism based on observation of children.[36] The Diagnostic interview for social and communication disorders (DISCO) may also be used.[91]
A pediatrician commonly performs a preliminary investigation by taking developmental history and physically examining the child. If warranted, diagnosis and evaluations are conducted with help from ASD specialists, observing and assessing cognitive, communication, family, and other factors using standardized tools, and taking into account any associated medical conditions.[92] A pediatric neuropsychologist is often asked to assess behavior and cognitive skills, both to aid diagnosis and to help recommend educational interventions.[93] A differential diagnosis for ASD at this stage might also consider intellectual disability, hearing impairment, and a specific language impairment[92] such as Landau–Kleffner syndrome.[94] The presence of autism can make it harder to diagnose coexisting psychiatric disorders such as depression.[95]
Clinical genetics evaluations are often done once ASD is diagnosed, particularly when other symptoms already suggest a genetic cause.[96] Although genetic technology allows clinical geneticists to link an estimated 40% of cases to genetic causes,[97] consensus guidelines in the US and UK are limited to high-resolution chromosome and fragile X testing.[96] A genotype-first model of diagnosis has been proposed, which would routinely assess the genome's copy number variations.[98] As new genetic tests are developed several ethical, legal, and social issues will emerge. Commercial availability of tests may precede adequate understanding of how to use test results, given the complexity of autism's genetics.[99] Metabolic and neuroimaging tests are sometimes helpful, but are not routine.[96]
ASD can sometimes be diagnosed by age 14 months, although diagnosis becomes increasingly stable over the first three years of life: for example, a one-year-old who meets diagnostic criteria for ASD is less likely than a three-year-old to continue to do so a few years later.[1] In the UK the National Autism Plan for Children recommends at most 30 weeks from first concern to completed diagnosis and assessment, though few cases are handled that quickly in practice.[92] Although the symptoms of autism and ASD begin early in childhood, they are sometimes missed; years later, adults may seek diagnoses to help them or their friends and family understand themselves, to help their employers make adjustments, or in some locations to claim disability living allowances or other benefits. Girls are often diagnosed later than boys.[100]
Underdiagnosis and overdiagnosis are problems in marginal cases, and much of the recent increase in the number of reported ASD cases is likely due to changes in diagnostic practices. The increasing popularity of drug treatment options and the expansion of benefits has given providers incentives to diagnose ASD, resulting in some overdiagnosis of children with uncertain symptoms. Conversely, the cost of screening and diagnosis and the challenge of obtaining payment can inhibit or delay diagnosis.[101] It is particularly hard to diagnose autism among the visually impaired, partly because some of its diagnostic criteria depend on vision, and partly because autistic symptoms overlap with those of common blindness syndromes or blindisms.[102]
Classification
Autism is one of the five pervasive developmental disorders (PDD), which are characterized by widespread abnormalities of social interactions and communication, and severely restricted interests and highly repetitive behavior.[29] These symptoms do not imply sickness, fragility, or emotional disturbance.[32]
Of the five PDD forms, Asperger syndrome is closest to autism in signs and likely causes; Rett syndrome and childhood disintegrative disorder share several signs with autism, but may have unrelated causes; PDD not otherwise specified (PDD-NOS; also called atypical autism) is diagnosed when the criteria are not met for a more specific disorder.[103] Unlike with autism, people with Asperger syndrome have no substantial delay in language development.[104] The terminology of autism can be bewildering, with autism, Asperger syndrome and PDD-NOS often called the autism spectrum disorders (ASD)[7] or sometimes the autistic disorders,[105] whereas autism itself is often called autistic disorder, childhood autism, or infantile autism. In this article, autism refers to the classic autistic disorder; in clinical practice, though, autism, ASD, and PDD are often used interchangeably.[96] ASD, in turn, is a subset of the broader autism phenotype, which describes individuals who may not have ASD but do have autistic-like traits, such as avoiding eye contact.[106]
The manifestations of autism cover a wide spectrum, ranging from individuals with severe impairments—who may be silent, developmentally disabled, and locked into hand flapping and rocking—to high functioning individuals who may have active but distinctly odd social approaches, narrowly focused interests, and verbose, pedantic communication.[107] Because the behavior spectrum is continuous, boundaries between diagnostic categories are necessarily somewhat arbitrary.[52] Sometimes the syndrome is divided into low-, medium- or high-functioning autism (LFA, MFA, and HFA), based on IQ thresholds,[108] or on how much support the individual requires in daily life; these subdivisions are not standardized and are controversial. Autism can also be divided into syndromal and non-syndromal autism; the syndromal autism is associated with severe or profound intellectual disability or a congenital syndrome with physical symptoms, such as tuberous sclerosis.[109] Although individuals with Asperger syndrome tend to perform better cognitively than those with autism, the extent of the overlap between Asperger syndrome, HFA, and non-syndromal autism is unclear.[110]
Some studies have reported diagnoses of autism in children due to a loss of language or social skills, as opposed to a failure to make progress, typically from 15 to 30 months of age. The validity of this distinction remains controversial; it is possible that regressive autism is a specific subtype,[15][44][1][111] or that there is a continuum of behaviors between autism with and without regression.[112]
Research into causes has been hampered by the inability to identify biologically meaningful subgroups within the autistic population[113] and by the traditional boundaries between the disciplines of psychiatry, psychology, neurology and pediatrics.[114] Newer technologies such as fMRI and diffusion tensor imaging can help identify biologically relevant phenotypes (observable traits) that can be viewed on brain scans, to help further neurogenetic studies of autism;[115] one example is lowered activity in the fusiform face area of the brain, which is associated with impaired perception of people versus objects.[20] It has been proposed to classify autism using genetics as well as behavior.[116]
Screening
About half of parents of children with ASD notice their child's unusual behaviors by age 18 months, and about four-fifths notice by age 24 months.[1] According to an article, failure to meet any of the following milestones "is an absolute indication to proceed with further evaluations. Delay in referral for such testing may delay early diagnosis and treatment and affect the long-term outcome".[33]
No response to name (or eye-to-eye gaze) by 6 months.[117]
No babbling by 12 months.
No gesturing (pointing, waving, etc.) by 12 months.
No single words by 16 months.
No two-word (spontaneous, not just echolalic) phrases by 24 months.
Loss of any language or social skills, at any age.
The United States Preventive Services Task Force in 2016 found it was unclear if screening was beneficial or harmful among children in whom there is no concerns.[118] The Japanese practice is to screen all children for ASD at 18 and 24 months, using autism-specific formal screening tests. In contrast, in the UK, children whose families or doctors recognize possible signs of autism are screened. It is not known which approach is more effective.[20] Screening tools include the Modified Checklist for Autism in Toddlers (M-CHAT), the Early Screening of Autistic Traits Questionnaire, and the First Year Inventory; initial data on M-CHAT and its predecessor, the Checklist for Autism in Toddlers (CHAT), on children aged 18–30 months suggests that it is best used in a clinical setting and that it has low sensitivity (many false-negatives) but good specificity (few false-positives).[1] It may be more accurate to precede these tests with a broadband screener that does not distinguish ASD from other developmental disorders.[119] Screening tools designed for one culture's norms for behaviors like eye contact may be inappropriate for a different culture.[120] Although genetic screening for autism is generally still impractical, it can be considered in some cases, such as children with neurological symptoms and dysmorphic features.[121]
Prevention
Management

A three-year-old with autism points to fish in an aquarium, as part of an experiment on the effect of intensive shared-attention training on language development.[124]
The main goals when treating children with autism are to lessen associated deficits and family distress, and to increase quality of life and functional independence. In general, higher IQs are correlated with greater responsiveness to treatment and improved treatment outcomes.[125][126] No single treatment is best and treatment is typically tailored to the child's needs.[7] Families and the educational system are the main resources for treatment.[20] Services should be carried out by behavior analysts, special education teachers, speech pathologists, and licensed psychologists. Studies of interventions have methodological problems that prevent definitive conclusions about efficacy.[127] However, the development of evidence-based interventions has advanced in recent years.[125] Although many psychosocial interventions have some positive evidence, suggesting that some form of treatment is preferable to no treatment, the methodological quality of systematic reviews of these studies has generally been poor, their clinical results are mostly tentative, and there is little evidence for the relative effectiveness of treatment options.[128] Intensive, sustained special education programs and behavior therapy early in life can help children acquire self-care, communication, and job skills,[7] and often improve functioning and decrease symptom severity and maladaptive behaviors;[129] claims that intervention by around age three years is crucial are not substantiated.[130] While medications have not been found to help with core symptoms, they may be used for associated symptoms, such as irritability, inattention, or repetitive behavior patterns.[10]
Education
Educational interventions often used include applied behavior analysis (ABA), developmental models, structured teaching, speech and language therapy, social skills therapy, and occupational therapy.[7] Among these approaches, interventions either treat autistic features comprehensively, or focalize treatment on a specific area of deficit.[125] The quality of research for early intensive behavioral intervention (EIBI)—a treatment procedure incorporating over thirty hours per week of the structured type of ABA that is carried out with very young children—is currently low, and more vigorous research designs with larger sample sizes are needed.[131] Two theoretical frameworks outlined for early childhood intervention include structured and naturalistic ABA interventions, and developmental social pragmatic models (DSP).[125] One interventional strategy utilizes a parent training model, which teaches parents how to implement various ABA and DSP techniques, allowing for parents to disseminate interventions themselves.[125] Various DSP programs have been developed to explicitly deliver intervention systems through at-home parent implementation. Despite the recent development of parent training models, these interventions have demonstrated effectiveness in numerous studies, being evaluated as a probable efficacious mode of treatment.[125]
Early, intensive ABA therapy has demonstrated effectiveness in enhancing communication, as well as adaptive and global functioning in preschool children;[132] it is well-established for improving the intellectual performance of that age group.[129] Similarly, a teacher-implemented intervention that utilizes a more naturalistic form of ABA combined with a developmental social pragmatic approach has been found to be beneficial in improving social-communication skills in young children, although there is less evidence in its treatment of global symptoms.[125] Neuropsychological reports are often poorly communicated to educators, resulting in a gap between what a report recommends and what education is provided.[93] It is not known whether treatment programs for children lead to significant improvements after the children grow up,[129] and the limited research on the effectiveness of adult residential programs shows mixed results.[133] The appropriateness of including children with varying severity of autism spectrum disorders in the general education population is a subject of current debate among educators and researchers.[134]
Medication
Medications may be used to treat ASD symptoms that interfere with integrating a child into home or school when behavioral treatment fails.[8] They may also be used for associated health problems, such as ADHD or anxiety.[8] More than half of US children diagnosed with ASD are prescribed psychoactive drugs or anticonvulsants, with the most common drug classes being antidepressants, stimulants, and antipsychotics.[11][12] The atypical antipsychotic drugs risperidone and aripiprazole are FDA-approved for treating associated aggressive and self-injurious behaviors.[10][32][135] However, their side effects must be weighed against their potential benefits, and people with autism may respond atypically.[10] Side effects, for example, may include weight gain, tiredness, drooling, and aggression.[10] SSRI antidepressants, such as fluoxetine and fluvoxamine, have been shown to be effective in reducing repetitive and ritualistic behaviors, while the stimulant medication methylphenidate is beneficial for some children with co-morbid inattentiveness or hyperactivity.[7] There is scant reliable research about the effectiveness or safety of drug treatments for adolescents and adults with ASD.[136] No known medication relieves autism's core symptoms of social and communication impairments.[137] Experiments in mice have reversed or reduced some symptoms related to autism by replacing or modulating gene function,[87][138] suggesting the possibility of targeting therapies to specific rare mutations known to cause autism.[86][139]
Alternative medicine
Although many alternative therapies and interventions are available, few are supported by scientific studies.[39][140] Treatment approaches have little empirical support in quality-of-life contexts, and many programs focus on success measures that lack predictive validity and real-world relevance.[41] Some alternative treatments may place the child at risk. The preference that children with autism have for unconventional foods can lead to reduction in bone cortical thickness with this being greater in those on casein-free diets, as a consequence of the low intake of calcium and vitamin D; however, suboptimal bone development in ASD has also been associated with lack of exercise and gastrointestinal disorders.[141] In 2005, botched chelation therapy killed a five-year-old child with autism.[142][143] Chelation is not recommended for people with ASD since the associated risks outweigh any potential benefits.[144] Another alternative medicine practice with no evidence is CEASE therapy, a mixture of homeopathy, supplements, and 'vaccine detoxing'.[145][146]
Although popularly used as an alternative treatment for people with autism, as of 2018 there is no good evidence to recommend a gluten- and casein-free diet as a standard treatment.[147][148][149] A 2018 review concluded that it may be a therapeutic option for specific groups of children with autism, such as those with known food intolerances or allergies, or with food intolerance markers. The authors analyzed the prospective trials conducted to date that studied the efficacy of the gluten- and casein-free diet in children with ASD (4 in total). All of them compared gluten- and casein-free diet versus normal diet with a control group (2 double blind randomized controlled trials, 1 double blind crossover trial, 1 single blind trial). In two of the studies, whose duration was 12 and 24 months, a significant improvement in ASD symptoms (efficacy rate 50%) was identified. In the other two studies, whose duration was 3 months, no significant effect was observed.[147] The authors concluded that a longer duration of the diet may be necessary to achieve the improvement of the ASD symptoms.[147] Other problems documented in the trials carried out include transgressions of the diet, small sample size, the heterogeneity of the participants and the possibility of a placebo effect.[149][150]
Prognosis
There is no known cure.[7][20] Children recover occasionally, so that they lose their diagnosis of ASD;[22] this occurs sometimes after intensive treatment and sometimes not. It is not known how often recovery happens;[129] reported rates in unselected samples have ranged from 3% to 25%.[22] Most children with autism acquire language by age five or younger, though a few have developed communication skills in later years.[157] Most children with autism lack social support, meaningful relationships, future employment opportunities or self-determination.[41] Although core difficulties tend to persist, symptoms often become less severe with age.[32]
Few high-quality studies address long-term prognosis. Some adults show modest improvement in communication skills, but a few decline; no study has focused on autism after midlife.[158] Acquiring language before age six, having an IQ above 50, and having a marketable skill all predict better outcomes; independent living is unlikely with severe autism.[159]
Epidemiology
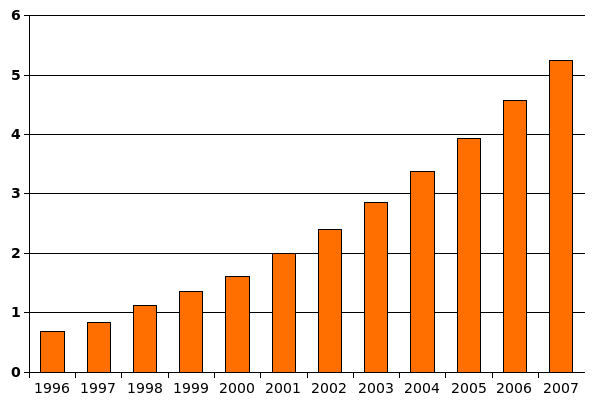
Reports of autism cases per 1,000 children grew dramatically in the US from 1996 to 2007. It is unknown how much, if any, growth came from changes in rates of autism.
Most recent reviews tend to estimate a prevalence of 1–2 per 1,000 for autism and close to 6 per 1,000 for ASD as of 2007.[25] A 2016 survey in the United States reported a rate of 25 per 1,000 children for ASD.[162] Globally, autism affects an estimated 24.8 million people as of 2015, while Asperger syndrome affects a further 37.2 million.[14] In 2012, the NHS estimated that the overall prevalence of autism among adults aged 18 years and over in the UK was 1.1%.[163] Rates of PDD-NOS's has been estimated at 3.7 per 1,000, Asperger syndrome at roughly 0.6 per 1,000, and childhood disintegrative disorder at 0.02 per 1,000.[164] CDC estimates about 1 out of 59 (1.7%) for 2014, an increase from 1 out of every 68 children (1.5%) for 2010.[165]
The number of reported cases of autism increased dramatically in the 1990s and early 2000s. This increase is largely attributable to changes in diagnostic practices, referral patterns, availability of services, age at diagnosis, and public awareness,[164][166] though unidentified environmental risk factors cannot be ruled out.[19] The available evidence does not rule out the possibility that autism's true prevalence has increased;[164] a real increase would suggest directing more attention and funding toward changing environmental factors instead of continuing to focus on genetics.[167]
Boys are at higher risk for ASD than girls. The sex ratio averages 4.3:1 and is greatly modified by cognitive impairment: it may be close to 2:1 with intellectual disability and more than 5.5:1 without.[25] Several theories about the higher prevalence in males have been investigated, but the cause of the difference is unconfirmed;[168] one theory is that females are underdiagnosed.[169]
Although the evidence does not implicate any single pregnancy-related risk factor as a cause of autism, the risk of autism is associated with advanced age in either parent, and with diabetes, bleeding, and use of psychiatric drugs in the mother during pregnancy.[168][170] The risk is greater with older fathers than with older mothers; two potential explanations are the known increase in mutation burden in older sperm, and the hypothesis that men marry later if they carry genetic liability and show some signs of autism.[28] Most professionals believe that race, ethnicity, and socioeconomic background do not affect the occurrence of autism.[171]
Several other conditions are common in children with autism.[20] They include:
Genetic disorders. About 10–15% of autism cases have an identifiable Mendelian (single-gene) condition, chromosome abnormality, or other genetic syndrome,[172] and ASD is associated with several genetic disorders.[173]
Intellectual disability. The percentage of autistic individuals who also meet criteria for intellectual disability has been reported as anywhere from 25% to 70%, a wide variation illustrating the difficulty of assessing intelligence of individuals on the autism spectrum.[174] In comparison, for PDD-NOS the association with intellectual disability is much weaker,[175] and by definition, the diagnosis of Asperger's excludes intellectual disability.[176]
Anxiety disorders are common among children with ASD; there are no firm data, but studies have reported prevalences ranging from 11% to 84%. Many anxiety disorders have symptoms that are better explained by ASD itself, or are hard to distinguish from ASD's symptoms.[177]
Epilepsy, with variations in risk of epilepsy due to age, cognitive level, and type of language disorder.[178]
Several metabolic defects, such as phenylketonuria, are associated with autistic symptoms.[179]
Minor physical anomalies are significantly increased in the autistic population.[180]
Preempted diagnoses. Although the DSM-IV rules out concurrent diagnosis of many other conditions along with autism, the full criteria for Attention deficit hyperactivity disorder (ADHD), Tourette syndrome, and other of these conditions are often present and these comorbid diagnoses are increasingly accepted.[181]
Sleep problems affect about two-thirds of individuals with ASD at some point in childhood. These most commonly include symptoms of insomnia such as difficulty in falling asleep, frequent nocturnal awakenings, and early morning awakenings. Sleep problems are associated with difficult behaviors and family stress, and are often a focus of clinical attention over and above the primary ASD diagnosis.[182]
History
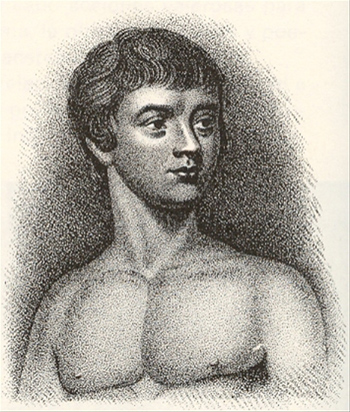
Portrait of Victor of Aveyron, a feral child caught in 1798 who displayed possible symptoms of autism[183]
A few examples of autistic symptoms and treatments were described long before autism was named. The Table Talk of Martin Luther, compiled by his notetaker, Mathesius, contains the story of a 12-year-old boy who may have been severely autistic.[184] Luther reportedly thought the boy was a soulless mass of flesh possessed by the devil, and suggested that he be suffocated, although a later critic has cast doubt on the veracity of this report.[185] The earliest well-documented case of autism is that of Hugh Blair of Borgue, as detailed in a 1747 court case in which his brother successfully petitioned to annul Blair's marriage to gain Blair's inheritance.[186] The Wild Boy of Aveyron, a feral child caught in 1798, showed several signs of autism; the medical student Jean Itard treated him with a behavioral program designed to help him form social attachments and to induce speech via imitation.[183]
The New Latin word autismus (English translation autism) was coined by the Swiss psychiatrist Eugen Bleuler in 1910 as he was defining symptoms of schizophrenia. He derived it from the Greek word autós (αὐτός, meaning "self"), and used it to mean morbid self-admiration, referring to "autistic withdrawal of the patient to his fantasies, against which any influence from outside becomes an intolerable disturbance".[187] A Soviet child psychiatrist, Grunya Sukhareva, described a similar syndrome that was published in Russian in 1925, and in German in 1926.[188]
Clinical development and diagnoses

Leo Kanner introduced the label early infantile autism in 1943.
The word autism first took its modern sense in 1938 when Hans Asperger of the Vienna University Hospital adopted Bleuler's terminology autistic psychopaths in a lecture in German about child psychology.[189] Asperger was investigating an ASD now known as Asperger syndrome, though for various reasons it was not widely recognized as a separate diagnosis until 1981.[183] Leo Kanner of the Johns Hopkins Hospital first used autism in its modern sense in English when he introduced the label early infantile autism in a 1943 report of 11 children with striking behavioral similarities.[46] Almost all the characteristics described in Kanner's first paper on the subject, notably "autistic aloneness" and "insistence on sameness", are still regarded as typical of the autistic spectrum of disorders.[63] It is not known whether Kanner derived the term independently of Asperger.[190]
Donald Triplett was the first person diagnosed with autism.[191] He was diagnosed by Kanner after being first examined in 1938, and was labeled as "case 1".[191] Triplett was noted for his savant abilities, particularly being able to name musical notes played on a piano and to mentally multiply numbers. His father, Oliver, described him as socially withdrawn but interested in number patterns, music notes, letters of the alphabet, and U.S. president pictures. By the age of 2, he had the ability to recite the 23rd Psalm and memorized 25 questions and answers from the Presbyterian catechism. He was also interested in creating musical chords.[192]
Kanner's reuse of autism led to decades of confused terminology like infantile schizophrenia, and child psychiatry's focus on maternal deprivation led to misconceptions of autism as an infant's response to "refrigerator mothers". Starting in the late 1960s autism was established as a separate syndrome.[193]
Terminology and distinction from schizophrenia
As late as the mid-1970s there was little evidence of a genetic role in autism; while in 2007 it was believed to be one of the most heritable psychiatric conditions.[194] Although the rise of parent organizations and the destigmatization of childhood ASD have affected how ASD is viewed,[183] parents continue to feel social stigma in situations where their child's autistic behavior is perceived negatively,[195] and many primary care physicians and medical specialists express some beliefs consistent with outdated autism research.[196]
It took until 1980 for the DSM-III to differentiate autism from childhood schizophrenia. In 1987, the DSM-III-R provided a checklist for diagnosing autism. In May 2013, the DSM-5 was released, updating the classification for pervasive developmental disorders. The grouping of disorders, including PDD-NOS, autism, Asperger syndrome, Rett syndrome, and CDD, has been removed and replaced with the general term of Autism Spectrum Disorders. The two categories that exist are impaired social communication and/or interaction, and restricted and/or repetitive behaviors.[197]
The Internet has helped autistic individuals bypass nonverbal cues and emotional sharing that they find difficult to deal with, and has given them a way to form online communities and work remotely.[198] Societal and cultural aspects of autism have developed: some in the community seek a cure, while others believe that autism is simply another way of being.[23][24][199]
Society and culture
An autistic culture has emerged, accompanied by the autistic rights and neurodiversity movements.[200][201][202] Events include World Autism Awareness Day, Autism Sunday, Autistic Pride Day, Autreat, and others.[203][204][205][206] Organizations dedicated to promoting awareness of autism include Autism Speaks, Autism National Committee, and Autism Society of America.[207] Social-science scholars study those with autism in hopes to learn more about "autism as a culture, transcultural comparisons... and research on social movements."[208] While most autistic individuals do not have savant skills, many have been successful in their fields.[209][210][211]
Autism rights movement
The autism rights movement is a social movement within the context of disability rights that emphasizes the concept of neurodiversity, viewing the autism spectrum as a result of natural variations in the human brain rather than a disorder to be cured.[202] The autism rights movement advocates for including greater acceptance of autistic behaviors; therapies that focus on coping skills rather than on imitating the behaviors of those without autism;[212] and the recognition of the autistic community as a minority group.[212][213] Autism rights or neurodiversity advocates believe that the autism spectrum is genetic and should be accepted as a natural expression of the human genome. This perspective is distinct from two other likewise distinct views: the medical perspective, that autism is caused by a genetic defect and should be addressed by targeting the autism gene(s), and fringe theories that autism is caused by environmental factors such as vaccines.[202] A common criticism against autistic activists is that the majority of them are "high-functioning" or have Asperger syndrome and do not represent the views of "low-functioning" autistic people.[213]
Employment
About half of autistics are unemployed, and one third of those with graduate degrees may be unemployed.[214] Among autistics who find work, most are employed in sheltered settings working for wages below the national minimum.[215] While employers state hiring concerns about productivity and supervision, experienced employers of autistics give positive reports of above average memory and detail orientation as well as a high regard for rules and procedure in autistic employees.[214] A majority of the economic burden of autism is caused by decreased earnings in the job market.[216] Some studies also find decreased earning among parents who care for autistic children.[217][218]