Wolff–Parkinson–White syndrome
Wolff–Parkinson–White syndrome
| Wolff–Parkinson–White syndrome | |
|---|---|
| Other names | WPW pattern, Ventricular pre-excitation with arrhythmia, auriculoventricular accessory pathway syndrome[1][2] |
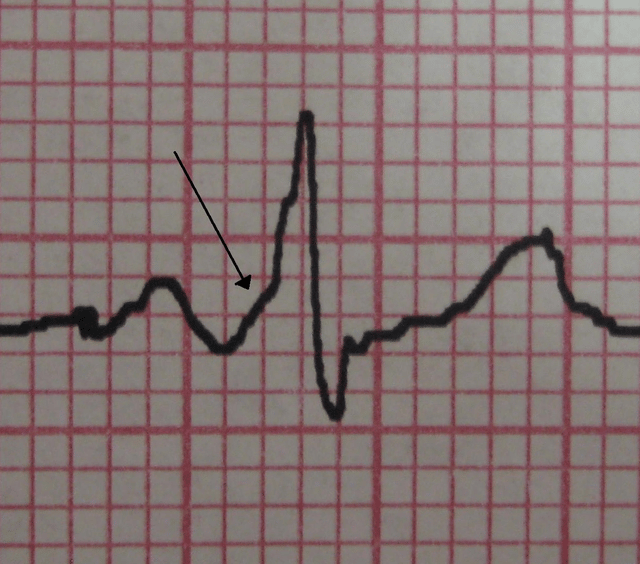
| A characteristic "delta wave" seen in a person with Wolff–Parkinson–White syndrome. Note the short PR interval. | |
| Specialty | Cardiology |
| Symptoms | Abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, loss of consciousness[1][2] |
| Complications | Cardiomyopathy, stroke, sudden cardiac death[2] |
| Usual onset | Birth[1] |
| Causes | Accessory pathway in the heart[1] |
| Diagnostic method | Electrocardiogram shows a short PR interval and delta wave[3] |
| Treatment | Watchful waiting, medications, radiofrequency catheter ablation[4][5] |
| Prognosis | Without symptoms 0.5% (children), 0.1% (adults) risk of death per year[5] |
| Frequency | 0.2%[1] |
Wolff–Parkinson–White syndrome (WPWS) is a disorder due to a specific type of problem with the electrical system of the heart which has resulted in symptoms.[2][3] About 40% of people with the electrical problem never develop symptoms.[5] Symptoms can include an abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, or syncope.[1] Rarely, cardiac arrest may occur.[1] The most common type of irregular heartbeat that occurs is known as paroxysmal supraventricular tachycardia.[1]
The cause of WPW is typically unknown.[2] A small number of cases are due to a mutation of the PRKAG2 gene which may be inherited from a person's parents in an autosomal dominant fashion.[2] The underlying mechanism involves an accessory electrical conduction pathway between the atria and the ventricles.[1] It is associated with other conditions such as Ebstein anomaly and hypokalemic periodic paralysis.[1] Diagnosis is typically when an electrocardiogram (ECG) show a short PR interval and a delta wave.[3] It is a type of pre-excitation syndromes.[3]
WPW syndrome is treated with either medications or radiofrequency catheter ablation.[4] It affects between 0.1 and 0.3% in the population.[1] The risk of death in those without symptoms is about 0.5% per year in children and 0.1% per year in adults.[5] In those without symptoms ongoing observation may be reasonable.[5] In those with WPW complicated by atrial fibrillation, cardioversion or the medication procainamide may be used.[6] The condition is named after Louis Wolff, John Parkinson, and Paul Dudley White who described the ECG findings in 1930.[3]
| Wolff–Parkinson–White syndrome | |
|---|---|
| Other names | WPW pattern, Ventricular pre-excitation with arrhythmia, auriculoventricular accessory pathway syndrome[1][2] |
| A characteristic "delta wave" seen in a person with Wolff–Parkinson–White syndrome. Note the short PR interval. | |
| Specialty | Cardiology |
| Symptoms | Abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, loss of consciousness[1][2] |
| Complications | Cardiomyopathy, stroke, sudden cardiac death[2] |
| Usual onset | Birth[1] |
| Causes | Accessory pathway in the heart[1] |
| Diagnostic method | Electrocardiogram shows a short PR interval and delta wave[3] |
| Treatment | Watchful waiting, medications, radiofrequency catheter ablation[4][5] |
| Prognosis | Without symptoms 0.5% (children), 0.1% (adults) risk of death per year[5] |
| Frequency | 0.2%[1] |
Signs and symptoms
People with WPW are usually asymptomatic when not having a fast heart rate. However, individuals may experience palpitations, dizziness, shortness of breath, or infrequently syncope (fainting or near fainting) during episodes of supraventricular tachycardia. The telltale "delta wave" may sometimes be seen on an electrocardiogram (ECG/EKG). WPW is also associated with a very small risk of sudden death due to more dangerous heart rhythm disturbances.[7]
Pathophysiology

Graphic representation of the electrical conduction system of the human heart
Transmission of a cardiac action potential through the conduction system of the normal human heart
Electrical activity in the normal human heart begins when a cardiac action potential arises in the sinoatrial (SA) node, which is located in the right atrium. From there, the electrical stimulus is transmitted via internodal pathways to the atrioventricular (AV) node. After a brief delay at the AV node, the stimulus travels through the bundle of His to the left and right bundle branches and then to the Purkinje fibers and the endocardium at the apex of the heart, then finally to the ventricular myocardium.
The AV node serves an important function as a "gatekeeper", limiting the electrical activity that reaches the ventricles. In situations where the atria generate excessively rapid electrical activity (such as atrial fibrillation or atrial flutter), the AV node limits the number of signals conducted to the ventricles. For example, if the atria are electrically activated at 300 beats per minute, half those electrical impulses may be blocked by the AV node, so that the ventricles are stimulated at only 150 beats per minute—resulting in a pulse of 150 beats per minute. Another important property of the AV node is that it slows down individual electrical impulses. This is manifested on the electrocardiogram as the PR interval (the time from electrical activation of the atria to electrical activation of the ventricles), which is usually shortened to less than 120 milliseconds in duration.
Individuals with WPW have an accessory pathway that communicates between the atria and the ventricles, in addition to the AV node. This accessory pathway is known as the bundle of Kent. This accessory pathway does not share the rate-slowing properties of the AV node, and may conduct electrical activity at a significantly higher rate than the AV node. For instance, in the example above, if an individual had an atrial rate of 300 beats per minute, the accessory bundle may conduct all the electrical impulses from the atria to the ventricles, causing the ventricles to contract at 300 beats per minute. Extremely rapid heart rates such as this may result in hemodynamic instability or cardiogenic shock. In some cases, the combination of an accessory pathway and abnormal heart rhythms can trigger ventricular fibrillation, a leading cause of sudden cardiac death.
Bundle of Kent
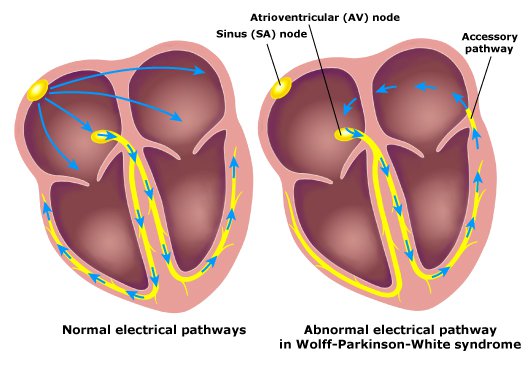
Graphic representation of the bundle of Kent in Wolff–Parkinson–White syndrome
The bundle of Kent is an abnormal extra or accessory conduction pathway between the atria and ventricles that is present in a small percentage (between 0.1 and 0.3%) of the general population.[9][10][11] This pathway may communicate between the left atrium and the left ventricle, in which case it is termed a "type A pre-excitation", or between the right atrium and the right ventricle, in which case it is termed a "type B pre-excitation".[12] Problems arise when this pathway creates an electrical circuit that bypasses the AV node. The AV node is capable of slowing the rate of conduction of electrical impulses to the ventricles, whereas the bundle of Kent lacks this capability. When an aberrant electrical connection is made via the bundle of Kent, tachydysrhythmias may therefore result.
Diagnosis
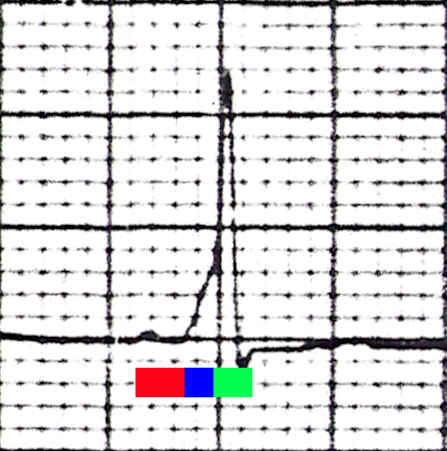
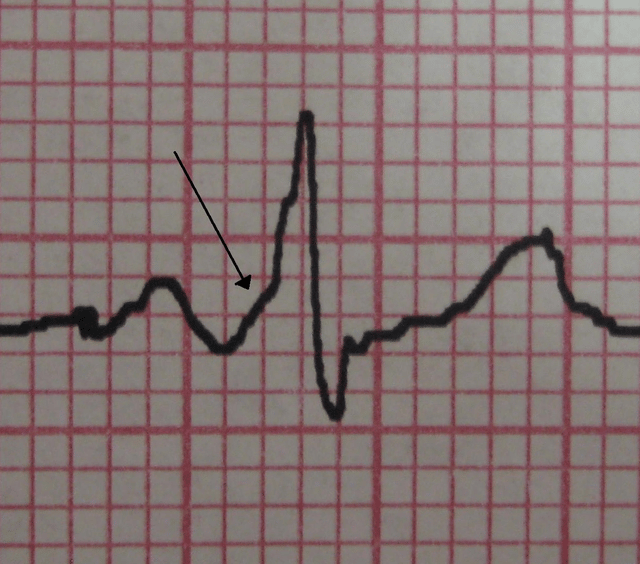
One beat from a rhythm strip in V2 demonstrating characteristic findings in Wolff–Parkinson–White syndrome: Note the characteristic delta wave (above the blue bar), the short PR interval (red bar) of 80 ms, and the long QRS complex (blue bar plus green bar) at 120 ms.
WPW is commonly diagnosed on the basis of the electrocardiogram in an asymptomatic individual. In this case, it is manifested as a delta wave, which is a slurred upstroke in the QRS complex that is associated with a short PR interval. The short PR interval and slurring of the QRS complex are reflective of the impulse making it to the ventricles early (via the accessory pathway) without the usual delay experienced in the AV node.
If a person with WPW experiences episodes of atrial fibrillation, the ECG shows a rapid polymorphic wide-complex tachycardia (without torsades de pointes). This combination of atrial fibrillation and WPW is considered dangerous, and most antiarrhythmic drugs are contraindicated.
When an individual is in normal sinus rhythm, the ECG characteristics of WPW are a short PR interval (less than 120 milliseconds in duration), widened QRS complex (greater than 120 milliseconds in duration) with slurred upstroke of the QRS complex, and secondary repolarization changes (reflected in ST segment-T wave changes).
In individuals with WPW, electrical activity that is initiated in the SA node travels through the accessory pathway, as well as through the AV node to activate the ventricles via both pathways. Since the accessory pathway does not have the impulse slowing properties of the AV node, the electrical impulse first activates the ventricles via the accessory pathway, and immediately afterwards via the AV node. This gives the short PR interval and slurred upstroke of the QRS complex known as the delta wave.
In case of type A pre-excitation (left atrioventricular connections), a positive R wave is seen in V1 ("positive delta") on the precordial leads of the electrocardiogram, while in type B pre-excitation (right atrioventricular connections), a predominantly negative delta wave is seen in lead V1 ("negative delta").[12]
People with WPW may have more than one accessory pathway—in some cases, as many as eight abnormal pathways have been found. This has been seen in individuals with Ebstein's anomaly.
Wolff–Parkinson–White syndrome is sometimes associated with Leber's hereditary optic neuropathy, a form of mitochondrial disease.[13]
Risk stratification
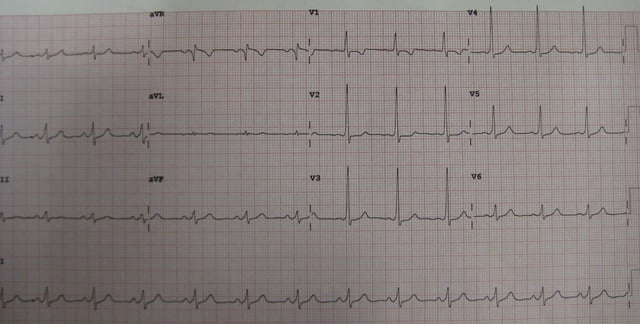
12 lead electrocardiogram of an individual with Wolff–Parkinson–White syndrome
WPW carries a small risk of sudden death, presumably due to rapidly conducted atrial fibrillation causing ventricular fibrillation. While the overall risk is approximately 2.4 per 1000 person years, the risk in an individual is dependent on the properties of the accessory pathway causing pre-excitation.[7]
A higher risk accessory pathway may be suggested by a history of syncope, but risk stratification is best performed by assessing how frequently a pathway can conduct impulse to the ventricles, usually via programmed electrical stimulation (PES) in the cardiac electrophysiology laboratory. This is an invasive but generally low-risk procedure during which the atria are stimulated to try to induce tachycardia. If a tachycardia involving the accessory pathway can be triggered, the cardiologist can then assess how rapidly the accessory pathway is able to conduct. The faster it can conduct, the higher the likelihood the accessory pathway can conduct fast enough to trigger a lethal tachycardia.
Risk stratification is best performed via programmed electrical stimulation (PES) in the cardiac electrophysiology laboratory. This is an invasive but generally low-risk procedure during which the atria are stimulated to try to induce tachycardia. If a tachycardia involving the accessory pathway can be triggered, the cardiologist can then assess how rapidly the accessory pathway is able to conduct. The faster it can conduct, the higher the likelihood the accessory pathway can conduct fast enough to trigger a lethal tachycardia.
High-risk features that may be present during PES include an effective refractory period of the accessory pathway less than 250 ms, multiple pathways, septal location of pathway, and inducibility of supraventricular tachycardia (AVRT, atrial fibrillation). Individuals with any of these high-risk features are generally considered at increased risk for SCD or symptomatic tachycardia, and should be treated accordingly (i.e.: catheter ablation).[14]
It is unclear whether invasive risk stratification (with PES) is necessary in the asymptomatic individual.[15] While some groups advocate PES for risk stratification in all individuals under 35 years old, others only offer it to individuals who have history suggestive of a tachydysrhythmia, since the incidence of sudden cardiac death is so low (less than 0.6% in some reports).[11][16][17]
Other methods of risk stratification include observing the ventricular rate during spontaneous atrial fibrillation on a 12-lead ECG. RR intervals of less than 250 ms suggest a higher risk pathway. During exercise testing, abrupt loss of pre-excitation as heart rate increases also suggest a lower risk pathway.[7] However, this approach is hampered by the normal improvement in AV node conduction during exercise which can also mask pre-excitation despite ongoing conduction down the accessory pathway.[18]
Treatment
People with WPW who are experiencing tachydysrhythmias may require synchronized electrical cardioversion if they are demonstrating severe signs or symptoms (for example, low blood pressure or lethargy with altered mental status). If they are relatively stable, medication may be used.
Medications
People with atrial fibrillation and rapid ventricular response are often treated with amiodarone[19] or procainamide[20] to stabilize their heart rate. Procainamide and cardioversion are now accepted treatments for conversion of tachycardia found with WPW.[21] Amiodarone was previously thought to be safe in atrial fibrillation with WPW, but after several cases of ventricular fibrillation, it is no longer recommended in this clinical scenario.[22]
AV node blockers should be avoided in atrial fibrillation and atrial flutter with WPW or history of it; this includes adenosine, diltiazem, verapamil, other calcium channel blockers, and beta blockers.[23] They can exacerbate the syndrome by blocking the heart's normal electrical pathway (therefore favoring 1:1 atrial to ventricle conduction through the pre-excitation pathway, potentially leading to unstable ventricular arrhythmias).
Radiofrequency catheter ablation
The definitive treatment of WPW is the destruction of the abnormal electrical pathway by radiofrequency catheter ablation. This procedure is performed by cardiac electrophysiologists. Radiofrequency catheter ablation is not performed in all individuals with WPW because inherent risks are involved in the procedure. When performed by an experienced electrophysiologist, radiofrequency ablation has a high success rate.[24] Findings from 1994 indicate success rates of as high as 95% in people treated with radiofrequency catheter ablation for WPW.[25] If radiofrequency catheter ablation is successfully performed, the condition is generally considered cured. Recurrence rates are typically less than 5% after a successful ablation.[24] The one caveat is that individuals with underlying Ebstein's anomaly may develop additional accessory pathways during progression of their disease.
History
In 1915, Frank Norman Wilson (1890–1952) became the first to describe the condition later called Wolff–Parkinson–White syndrome.[28] Alfred M. Wedd (1887–1967) was the next to describe the condition in 1921.[29] Cardiologists Louis Wolff (1898–1972), John Parkinson (1885–1976) and Paul Dudley White (1886–1973) are credited with the definitive description of the disorder in 1930.[30]
Notable cases
LaMarcus Aldridge, American basketball player[31]
Michael Cera, Canadian actor[32]
Nathan Eagleton, former Australian rules football player[33]
Jeff Garlin, American actor, writer, and comedian[34]
Quentin Groves, American football player who died of a heart attack at age 32[35]
Dan Hardy, British UFC welterweight fighter,[36] turned analyst and commentator
Mitch Hurwitz, American television writer and producer, creator of Arrested Development[34]
Marilyn Manson, American musician, painter, and actor[38]
Meat Loaf, American musician[39]
Michael Rupp, American ice hockey player[40]
Montel Vontavious Porter, professional wrestler[41]
Michael Montgomery, American football player[42]
See also
Re-entry ventricular arrhythmia